12 Outdated Nursing Practices
By

Have you ever wondered what nurses do during the historic times? When mechanical ventilators are not yet invented, how do nurses manage to survive? Rather, did their patients back then survive?
Charles Darwin once said, “It is not the strongest of the species that survive, nor the most intelligent, but the one most responsive to change.”
Pondering upon this quote, we realize that the nursing profession survived because of our ability to adapt to changes. It is dynamic. Whatever innovation in nursing techniques we have not is because of how we embraced the evolution of healthcare.
Nightingale said: “Unless we are making progress in our nursing every year, every month, every week, take my word for it, we are going back.”
The past is important to move forward. And yes, we are entering a new era of nursing interventions.
Let’s hop in a time machine and travel back in time and learn about the practices we don’t do (hopefully for good) anymore.
1. Rotating tourniquets
Also known as congesting cuffs, are often used to treat patients with acute pulmonary edema secondary to heart failure during the 1960’s. The idea was topool the blood in the veins and decrease the venous return therefore ultimately decreasing pulmonary congestion. Congesting cuffs were placed on three extremities and inflated to 20 to 80 mmHg to achieve its effect.
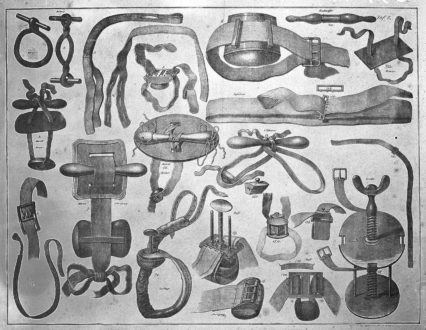 Tourniquet invented by Morell. Image via: commons.wikimedia.org
Tourniquet invented by Morell. Image via: commons.wikimedia.org
Why did it disappear? Aside from being time-consuming, potent drugs like diureticsare available today. Studies also cannot support the effectivity of this practice.
2. Use of the artificial lung: “The Iron Lung Machine.”
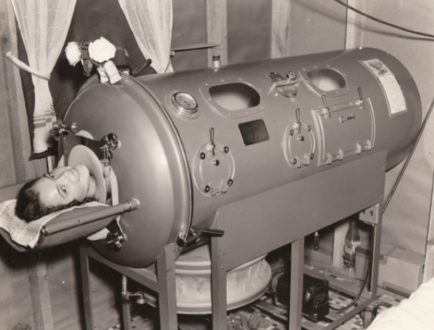 Colloquially known as the “iron lung,” enables a person to breathe when normal muscle control has been lost. It consisted of a large airtight tank in which the patient laid in, with his or her head sticking out.
Colloquially known as the “iron lung,” enables a person to breathe when normal muscle control has been lost. It consisted of a large airtight tank in which the patient laid in, with his or her head sticking out.
According to Wikipedia, the first of these devices to be widely used was developed by Drinker and Shaw in 1928. The iron lung often referred to in the early days as the “Drinker respirator,” was invented by Philip Drinker (1894–1972) and Louis Agassiz Shaw, Jr., professors of industrial hygiene at the Harvard School of Public Health.
 Iron lung ward filled with large number of polio patients, Rancho Los Amigos Hospital, California (1953)
Iron lung ward filled with large number of polio patients, Rancho Los Amigos Hospital, California (1953)
Some of the Iron Lung machines are still used in the US, but only a few extinct nurses know how to use them.
Why did it disappear? The use of modern treatment and portable ventilators including the eradication campaign against polio – the last case of naturally occurring polio happened in 1979 – sparked the decline of the iron lung machine.
3. Reuse of urinary catheters and syringes
 These were glass with a metal plunger. 10-20cc were used for blood taking and two ccs. For drug injection. Image via: http://samhs.org.au/
These were glass with a metal plunger. 10-20cc were used for blood taking and two ccs. For drug injection. Image via: http://samhs.org.au/
Back then, resterilization of syringes and urinary catheters were a trend. Syringes were made of glass and catheters were made of metal instead of the silicone we use today. Since they’re made of hardened materials, they were heat sterilized and immersed in alcohol– a practice that would be frowned upon today. Needles were not for single use and had to be sharpened manually. Yikes.
 Metal urinary catheters. Image via: http://samhs.org.au/
Metal urinary catheters. Image via: http://samhs.org.au/
Why did it disappear? Single use disposable syringes are the standard today ever since the occurrence of HIV and blood-borne pathogens. Different reusable equipment was produced because it’s safer and prevents cross contamination. Also, resterilizing is more costly for hospitals.
4. Notable antiseptic: Dakin’s Solution for wounds
Dakin’s solution was used mostly during the Worlds War I. It is composed of sodiumhypochlorite and baking soda, and invented by a chemist and a surgeon. After the war, it was widely used for bedsoresand infected wounds.
 Dakin’s Solution|healthykin.com
Dakin’s Solution|healthykin.com
Why did it disappear? It didn’t! Some institutions still use this today though others prefer proven antiseptics like povidone iodine, etc. But normal saline proves to be the best.
5. Penthrane and Trilene inhalers for labor pain
An inhaler for pain relief was once introduced for pregnant women who can’t tolerate labor pain.
 Analgizer. Image via: anaesthesiaheritagecentre
Analgizer. Image via: anaesthesiaheritagecentre
Trichloroethylene (Trilene) and methoxyflurane (Penthrane) were popular analgesics used in obstetrics during the 1900’s. These were administered via a calibrated, temperature-compensated vaporizers given to a mother for PRN painrelief during labor.
Why did it disappear? The drugs were effective for pain relief, so effective that they caused maternal sedation as well as neonatal depression. It also caused vomiting and accumulation causing renal damage. Due to its adverse effects, its use was discontinued.
6. Sliding scale insulin with urinedipstick results
Before the dawn of the great glucometer, nurses have to obtain a patient’s urinesample before meals to test for the presence of glucose.
Why did it disappear? Usage of the urinedipstick test was not longer recommended as glucometer devices provide a more accurate measurement of a patient’s glucose levels.
7. Antacid to pressure ulcers
A retired senior nurse recalled applying an antacid to pressure ulcer believing it would heal the wound faster.
Why did it disappear? It is now well known that moist wound healing is the ideal environment for faster healing, according to various studies.
8. Controlling foul wound odor with charcoal
Back then nurses used to dab teaspoons charcoal and wrap a gauze around an infected open wound to facilitate faster healing and to minimize the foul odor – thinking charcoal would absorb the odor.
 Leg wound treated with charcoal poultice.|charcoalremedies.com
Leg wound treated with charcoal poultice.|charcoalremedies.com
Why did it disappear? It didn’t. Actually, some people still use activated charcoalfor wounds thought the risk of infection is high on some instances.
9. Instilling saline solution to rinse mucus during suctioning.
It was then thought that saline acts as a lubricant in facilitating the ease of passage of the suction catheter with the same concept, it was also thought to loosen and dilute secretions and enhance a cough.
Why did it disappear? Instilling was often traumatic for patients, and cough reflexwas not always elicited especially for people with tetraplegia with little or nodiaphragm innervation. Prevalence of mucolytics to enhance mobilization of secretions is most commonly used. Studies have also proved that the practice increases the patient’s risk for pneumoniaand the possibility of pushing bacterial formation deeper into the lungs.
10. Cut the Foley catheter before removal.
An old-school practice that deserves to stay as it is. The practice involves snipping an inserted indwelling foley catheter to facilitate easy removal.
Why did it disappear? The practice can be considered dangerous because the tension can cause the end left with the patient to retract into the bladder.
11. Milking chest tube drains
This involves squeezing, twisting, or kneading the chest tube to create bursts of suction to move clots and remove any visible secretions.
Why did it disappear? The reason is therisk of air leakage within the chest tube, which can cause irritation and tissue trauma around the insertion site of the tubing.
12. Coca-Cola to unclog nasogastric tubes.
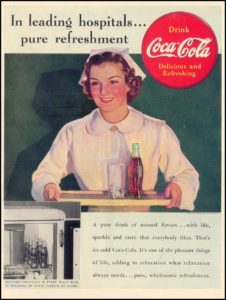 Image via Gallery of Graphic Design
Image via Gallery of Graphic Design
Coca-cola (or any carbonated soda) is a notorious unclogger for feeding tubes. The acidity in cola is believed help unclog the tube.
Why did it disappear? Coke, being an acidic fluid, can damage the integrity of the NG tube. It can also contribute to clogging by denaturing proteins in some enteral formulas. Water or replacing the tube isrecommended.
Knowing these interventions is a revelation for present nurses. Nevertheless, these practices taught us a lesson: to continually improve and render the best and proven care we could give to our patients.
I know many hospitals still practice number 3 till tomorrow in the name of cutting cost.
Which of the above practice did you do or still doing? Comment below and let the conversation begins!
Best wishes!











No comments:
Post a Comment